the pain project
How might we engage diverse patient and provider communities in the design of tools to help evaluate and better manage chronic pain?
Pain is a crisis. As many as 100 million Americans suffer from chronic pain. And although pain itself is a universal experience, it is difficult to communicate, and pain perception and communication vary across ages, genders, and cultures. Further, more than 2 million Americans suffer from an opioid use disorder—meaning they are addicted to prescription opioids—and about 90 Americans die every day from overdoses that involve an opioid.
At DiPi, we are partnering with primary care providers, pain experts, and public health officials throughout California to help address the challenging (and often personal and emotional) issues associated with this crisis. Our goal is to engage patient and provider communities in the participatory design of tools to help evaluate and better manage chronic pain—tools that invite discussion, create awareness about pain treatment options, encourage questions, help build trust, and work toward better health outcomes through shared decision-making and more effective doctor-patient communication.
This work is funded in part by a 2016-17 Sappi Ideas that Matter grant, awarded in support of projects where design can play an important role in helping to solve complex social issues. The materials we develop are open source, encouraging other healthcare stakeholders to adapt the information for local patient and provider needs.
opioid patient-education videos
Created with UC Davis Health / Opioid Task Force

Starting an opioid prescription requires each patient to have a thorough understanding of important and complicated information. Often there isn’t enough time to cover the safe use of these painkillers in a single appointment. To remedy this, we worked with the Opioid Task Force at UC Davis Medical Center to create a patient education video that covers important topics related to opioid risks, safety, and prescribing policies.
The seven-minute animation with music and voiceover reinforces the main points of the Patient-Prescriber Agreement (PPA) that patients typically sign before being prescribed opioids, and explains other important concepts such as the difference between dependence, tolerance, and addiction. Patients can view the video in exam rooms or online through MyChart, UC Davis Health System’s confidential way to access personal medical information and communicate with doctors.
An acute pain version, created by DiPi as part of a collaboration with the Society of Hospital Medicine (a network of more than 15,000 hospital medicine professionals), is aimed at reducing adverse drug events involving opioid medications and will be shown to patients prior to discharge from the hospital.
For the general public, a third version of the video is available on Youtube and linked to from the Sacramento County Department of Health and Human Services website. It includes subtitles in English, Spanish, Mandarin, and Hindi, with Tagalog, Vietnamese, and Russian to come.
Available under a Creative Commons Attribution-NonCommercial-NoDerivatives License, the videos have been adopted by clinics and hospitals nationwide.
Contact us to use these Opioid Patient-Education Videos or to adapt them to your local needs.
introduction to opioids booklet (video companion)
Created with UC Davis Health / Sacramento, CA + Hill Country Health and Wellness Center / Shasta County, CA
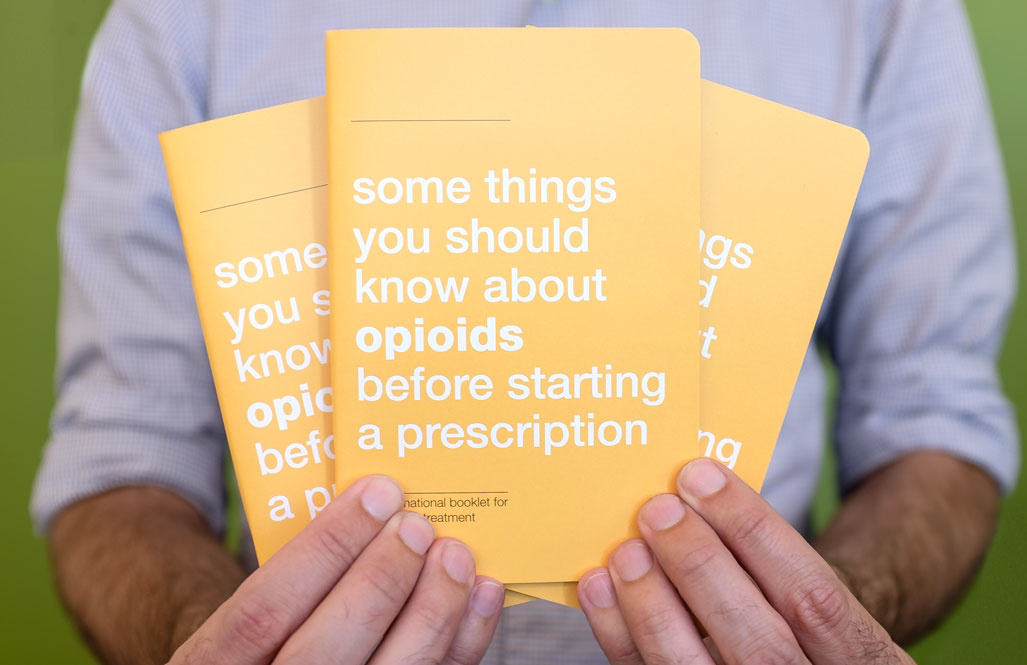

While some patients may prefer to view the opioid patient-education video more than once, not everyone has access to the internet or a digital device once they leave the clinic. By adapting the video into a pocket-sized 56-page booklet, we created a way for patients to easily take it home with them, share the information with friends and family, and reference it throughout their pain treatment.
Over 600 booklets have been printed and distributed to date.
Contact us to use the Introduction to Opioids Booklet under a Creative Commons license and adapt it to your local needs.
alternative treatments poster
Created with Hill Country Health and Wellness Center / Shasta County, CA

Hill Country Health and Wellness Center’s mission is to provide holistic care to patients. In support of this mission, we created an alternative treatments poster introducing patients to a variety of non-medication options for treating chronic pain, such as acupuncture, biofeedback, or physical therapy. Helping patients understand the potential benefits of different pain treatment options may reduce use, and therefore dependence on or addiction to, opioid medications. Poster graphics are color-coded for different kinds of information, providing patients with helpful tips related to different facets—emotional, physical, nutritional, and social—of an integrated pain management approach. Patients can view these posters while waiting to see their providers, and providers can refer to the poster during shared decision-making processes with patients. A mini version is available for patients to take home with them, or to print out.
Contact us to use the Alternative Treatments Poster under a Creative Commons license and adapt it to your local needs.
alternative treatments card deck
Created with Hill Country Health and Wellness Center / Shasta County, CA

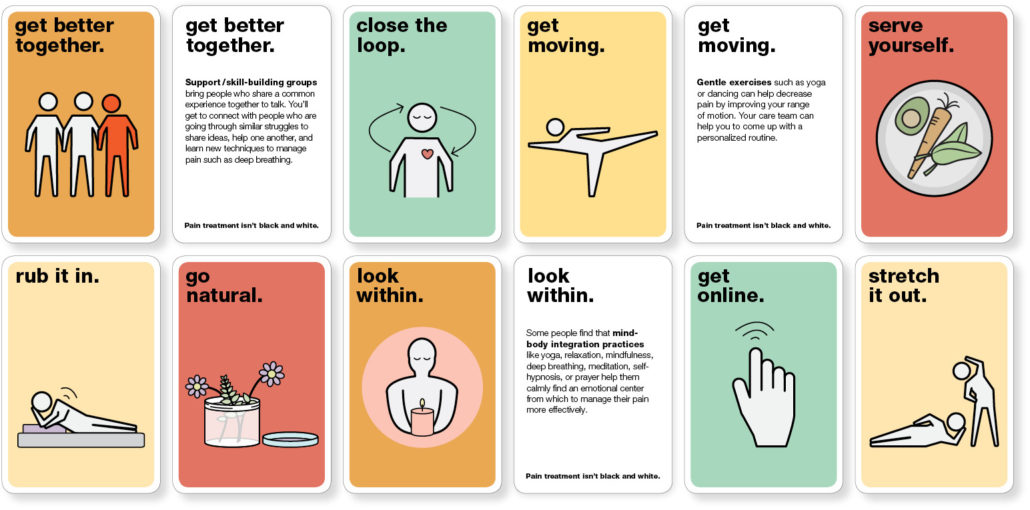
Patients often are unaware of the range of pain treatment options that exist and can miss the potential benefit of treatments due to this lack of knowledge. A companion piece to the poster and booklets, this deck of 16 cards (one per treatment option) is a shared-decision tool that providers can tailor to and integrate into their practice. The cards are being used at clinics including Hill Country Health and Wellness Center.
Contact us to use the Alternative Treatments Card Deck under a Creative Commons license and adapt it to your local needs.
opioid tapering booklet
Created with Hill Country Health & Wellness Center / Shasta County, CA
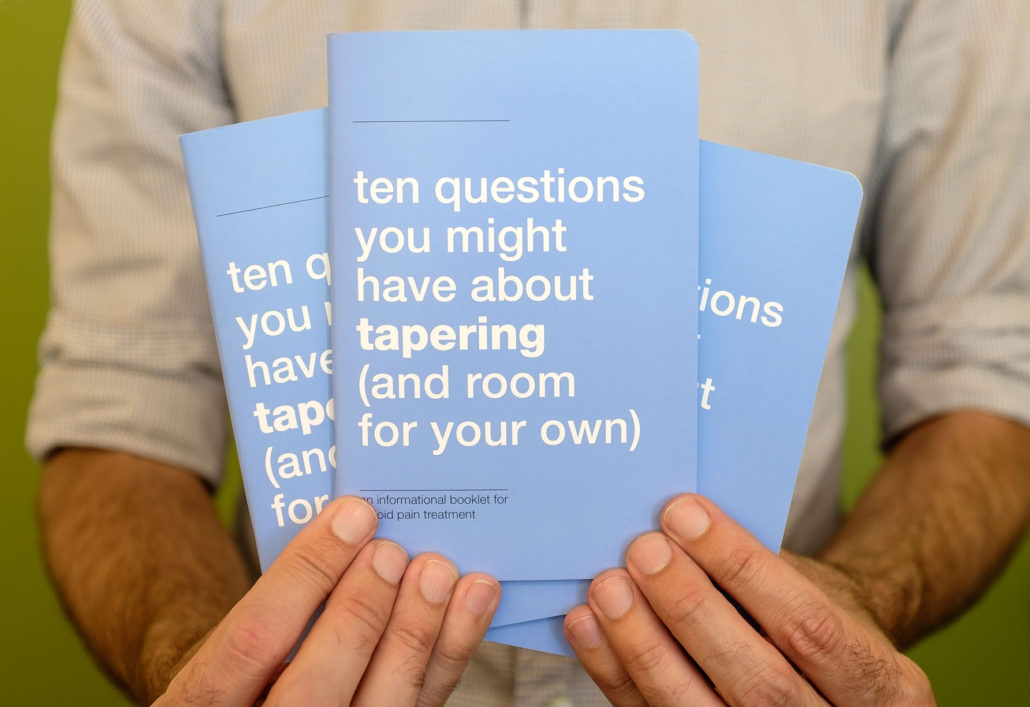
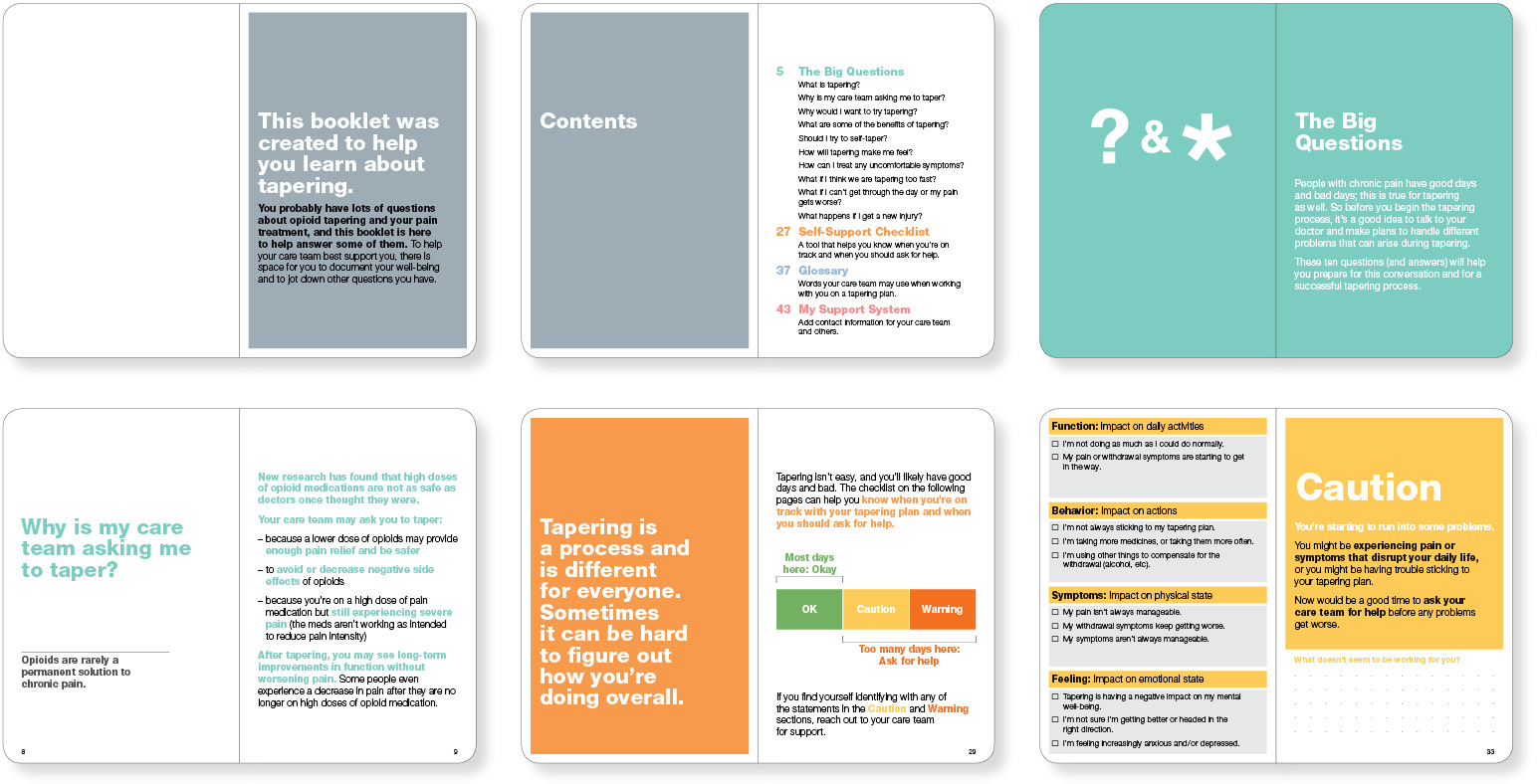
The idea of tapering can be scary for some patients—people living with chronic pain who use opioids as part of their pain management plan may fear that their medicine will be taken away “cold turkey.” This booklet normalizes tapering by providing a conversational way of introducing it when a patient starts using opioids or when they might reduce their dose or get off of opioids completely. It can be used between providers and their patients or between patients and their friends and family.
Integrating commonly asked questions and answers, a checklist to determine what is normal and when to ask for help, and a glossary of terms, this 56-page booklet educates and empowers patients in their own care. It may be used alone or along with the introduction-to-opioids booklet and the alternative treatment decision cards.
Contact us to use the Tapering Booklet under a Creative Commons license and adapt it to your local needs.
pain-treatment folder
Created with Hill Country Health and Wellness Center / Shasta County, CA
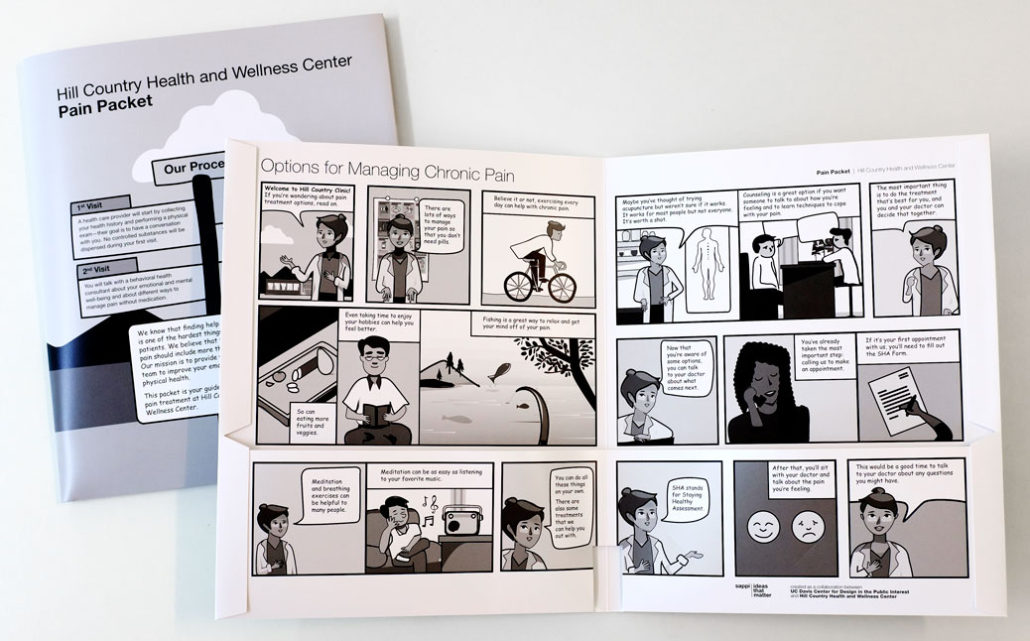
The pain treatment process can be confusing to navigate. What was originally a long text document has been reimagined as a friendly, welcoming outline of patient expectations and the logistics of treating chronic pain at Hill Country clinics in Shasta County, California. The pain-treatment folder outlines Hill Country’s care philosophy and illustrates the treatment process in the style of a comic book. Our goal is to humanize this confusing process and to help patients understand what to expect and what’s expected of them. We also hope that this approach may be of interest to other clinics or hospitals where patients can benefit from a better understanding of tests, surgical procedures, or treatment protocols.
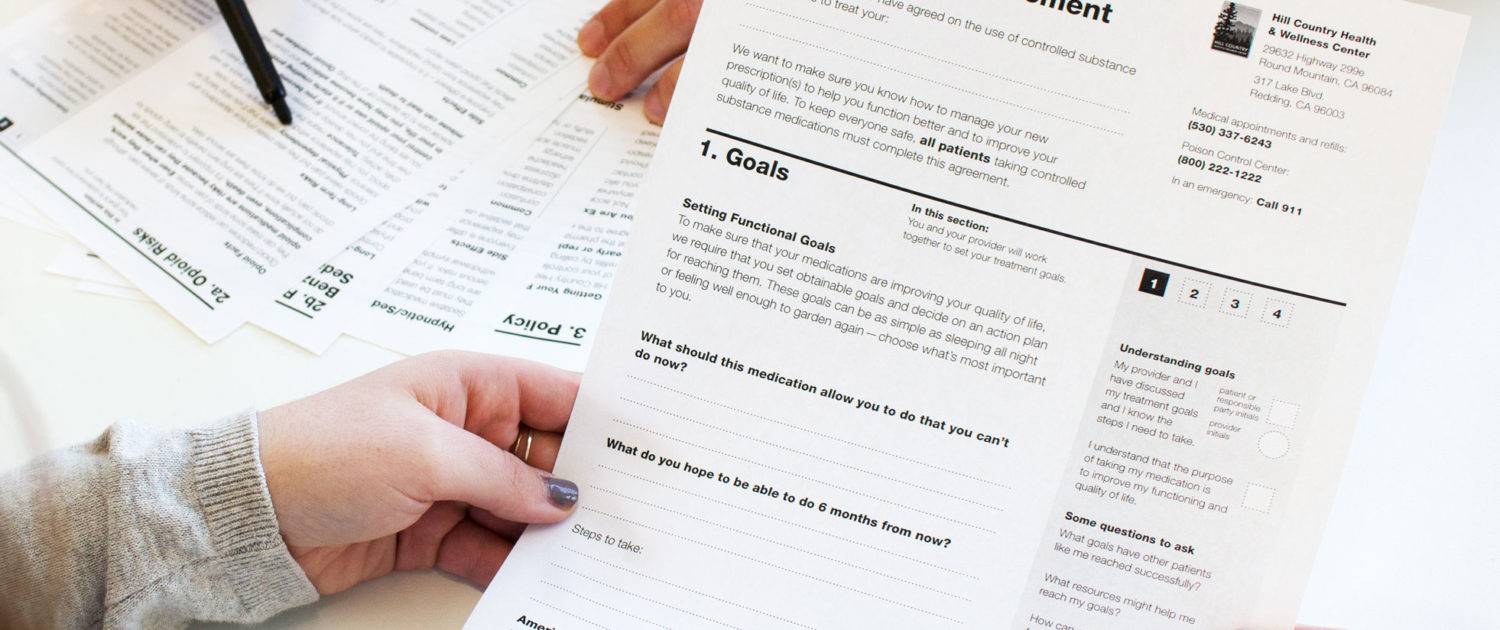
patient-prescriber agreement (PPA)
Created with UC Davis Health
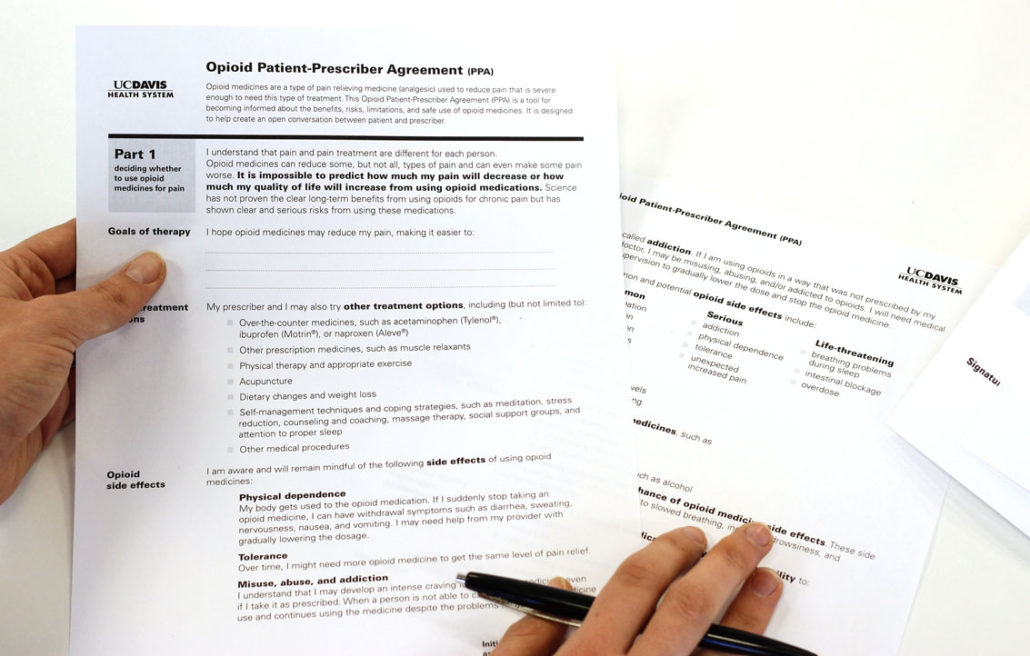
We are working with members of the Opioid Task Force at UC Davis Health System to design and implement a more patient-focused Patient-Prescriber Agreement (PPA), a document that patients sign to receive (or continue receiving) opioid medications. PPAs are part of a relatively recent change in opioid medication prescribing. While many PPAs are simply policy statements, well-designed agreements can do more, including serving as patient education tools; reducing strain and increasing trust between providers and patients; and helping patients understand opioid medications as part of an overall pain management strategy whose success is measured in terms of meeting functional goals.
Based on federal guidelines, the original UCD PPA looked somewhat dense and unwelcoming. With an aim to be as clear and user-friendly as possible, the DiPi team undertook a redesign in several phases—benchmarking to identify goals; editing and streamlining in a DiPi-led workshop; prototyping; reviews; and pilot testing. Due to the constraints of the electronic medical record system, the PPA had to be created in Rich Text Format, a daunting challenge.
Along with the patient-education video, created as a companion to the PPA, the redesign has been successfully integrated into UC Davis Health’s electronic medical record system and piloted at three primary care clinics (with a phased rollout to all 12 clinics beginning in summer 2017).
Contact us to use this Patient-Prescriber Agreement (PPA) under a Creative Commons license and adapt it to your local needs.
controlled substance and wellness agreement
Created with Hill Country Health and Wellness Center / Shasta County, CA
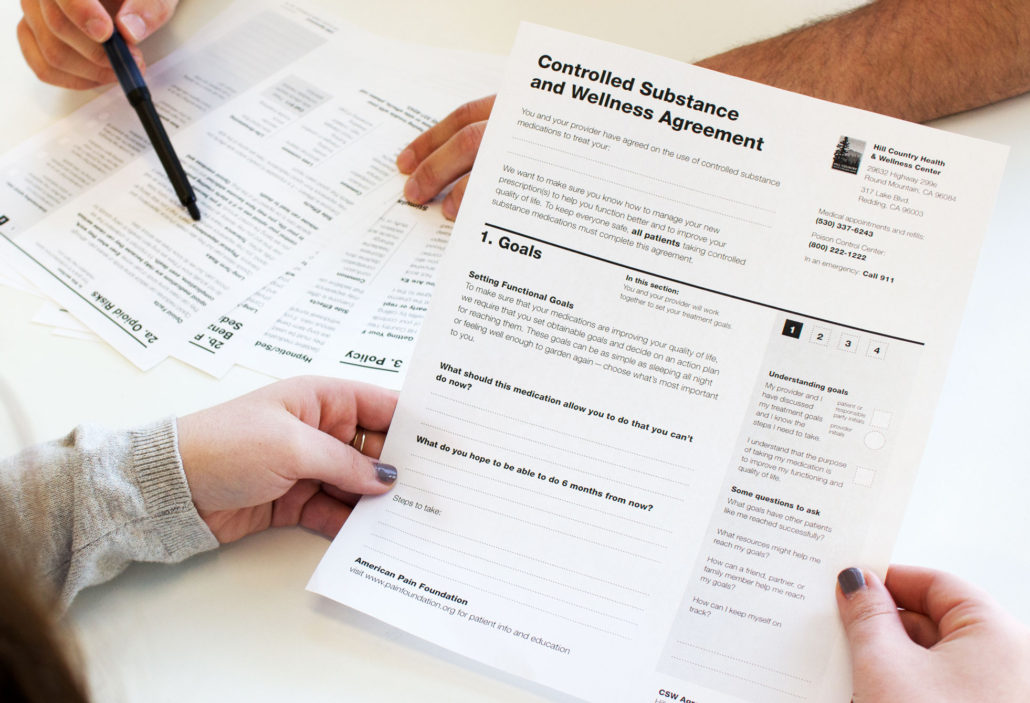
In collaboration with Hill Country Health and Wellness Center, we created a very different version of the Patient-Prescriber Agreement (also called a Controlled Substance Wellness Agreement), one that is designed to help patients slow down, reflect, and record questions and notes to discuss with their provider. Our process included relationship-building through multiple site visits, benchmarking via a provider survey and discussions, analysis of findings (e.g. mapping patient experiences and document flow at Hill Country), literature reviews, content development, iterative prototyping, user testing, and revision. We focused on how the specific needs, constraints, and opportunities at Hill Country might be addressed in the patient-centered content and design of the PPA. This includes chunking information into manageable sections, creating a strong information hierarchy, clearly calling out key points, and providing a quick-read zone and space to jot down questions. Content is written in plain language with a welcoming tone.
The new PPA was implemented at Hill Country clinics in Redding and Round Mountain beginning in fall 2016. We are now testing it in a quasi-experimental study to determine if the redesign does, in fact, have the intended effects. The ongoing study involves research, development, and design of a patient survey, assessment methods, development of IRB protocols, and, at Hill Country, a workshop presenting the study plan and a training session for clinic staff. We have collected 75 patient surveys and are currently analyzing the results.
While the PPA is one artifact, it represents a larger system of patient communication tools we are developing with Hill Country and has led to partnering with them on efforts to extend the project to as many as 14 counties in California.
Contact us to use the Controlled Substance and Wellness Agreement under a Creative Commons license and adapt it to your local needs.
opioid conversion tools
Created with UC Davis Health

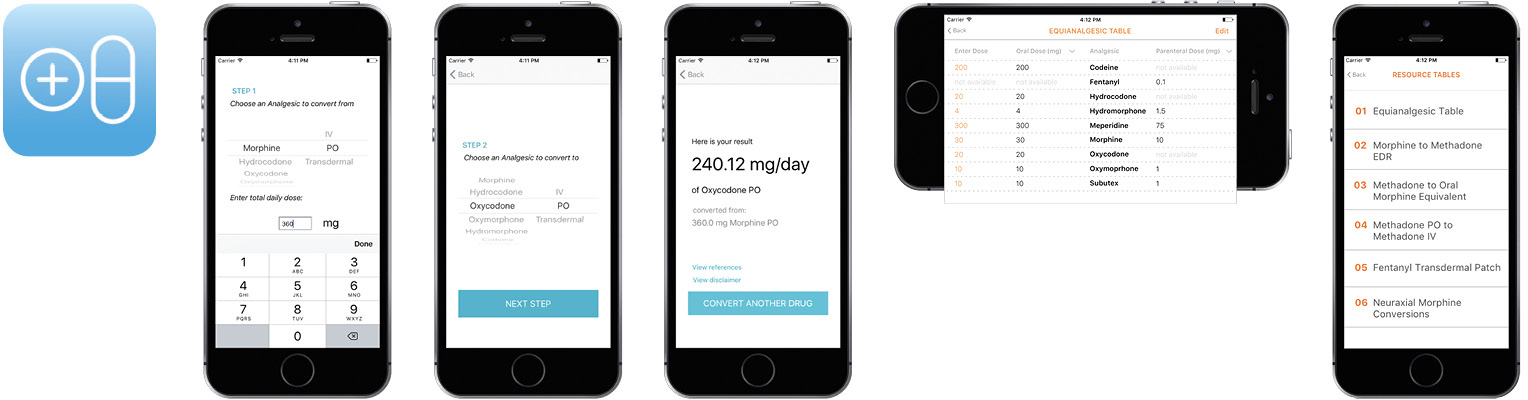
Patients who take opioid medications sometimes need to change from one medication to another. We are developing conversion tools to help providers adjust opioid dosages and/or find equivalent medications. These materials, including a one-page handout, a set of pocket-sized cards, and a prototype smartphone app, will make it easier for doctors to quickly find conversion ratios and adjust prescriptions. Because the calculations are based on local best practices, the opioid conversion tools will also increase newer physicians’ confidence and comfort with making conversions.
outpatient radio
Created with Hill Country Health and Wellness Center / Shasta County, CA
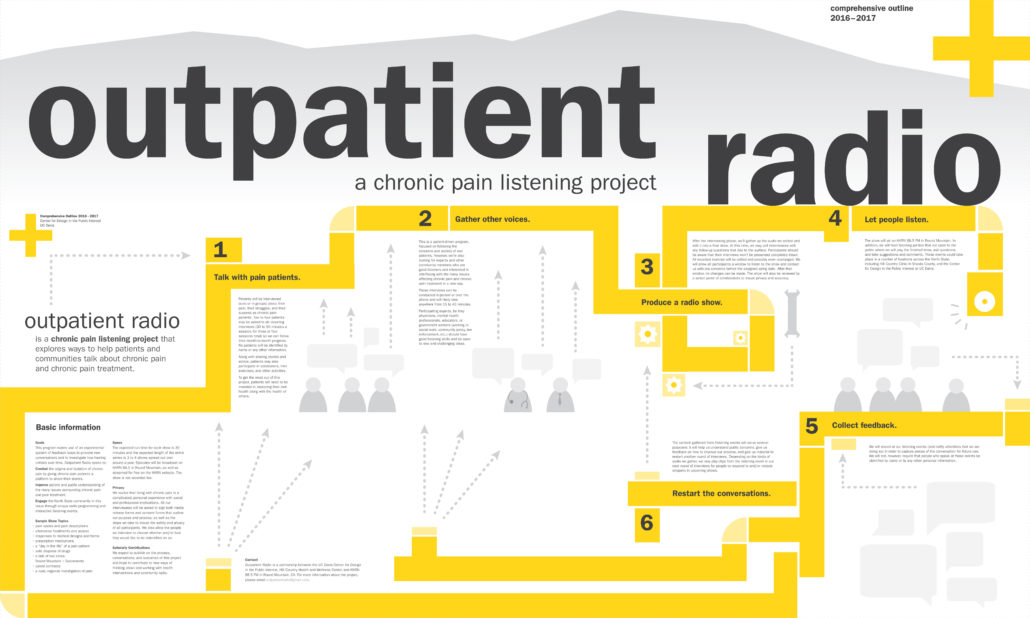
Outpatient Radio is a participatory community radio show produced in collaboration with Hill Country Health and Wellness Center and with support from Art Rx and Crocker Art Museum. Weaving together the stories of eight chronic pain patients from Solano, Sacramento, and Shasta Counties, the program explores ways to help patients and communities talk about chronic pain and chronic pain treatment. Through collecting and sharing stories in-person, on-air, and online, we are exploring how narratives connect, inform, and support communities through listening and conversation.
pain project: DiPi team
Susan Verba
Faculty, Design
Sarah Perrault
Faculty, University Writing Program
Bo Feng
Faculty, Communication
George Slavik
Graduate student, Design
Patrice Ehlert
Graduate student, Design
Vega Sood
Translator, opioid patient-education video
Lana Kazakova
Translator, opioid patient-education video
Kenna Fallan
Research/design staff
Tracy Manuel
Research/design staff
Karyn Kershaw
Research/design staff
Nima Rahni
Research/design staff
Yuting Han
Intern, mobile app development
Marc Holtsman
Intern, mobile app development
Emily Alameida
Undergraduate assistant
Chelsea Best
Undergraduate assistant
Thea Kaiser
Undergraduate assistant
Michelle Lee
Undergraduate assistant
Zoe Martin
Undergraduate assistant
Elisa Massenzio
Undergraduate assistant
Jazmin Valencia
Undergraduate assistant
pain project: community partners + participants
Physicians, patients, pharmacists, and clinician/researchers at UC Davis Health
Sacramento, CA
Clinicians, staff, patients, and community volunteers at Hill Country Health and Wellness Center